Top Articles

Trump admin pursues immigration charges in fatal crash case

Beyoncé to commence Cowboy Carter Tour at SoFi

US News
See all »China vows to counter Trump’s ‘bullying’ tariffs as global trade war escalates

Key takeaways from Trump’s ‘Liberation Day’ tariffs
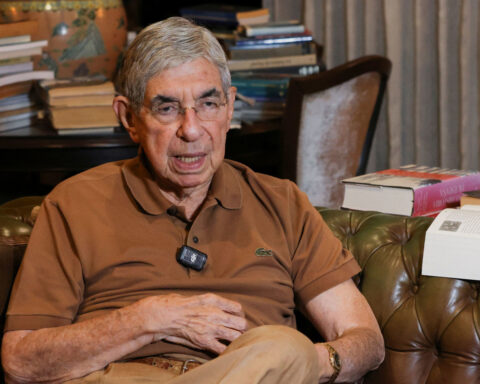
Former Costa Rican president who compared Trump to ‘Roman emperor’ says US has revoked his visa
‘The most powerful type of liar’: Tapper asks Anna Delvey how she views her criminal past
World News
See all »Trump and Zelenskiy meet one-on-one in Vatican basilica to seek Ukraine peace

Former Costa Rican president who compared Trump to ‘Roman emperor’ says US has revoked his visa
The Taliban senses an opening as it pushes for diplomatic recognition in talks with Trump administration

World leaders react to Trump's tariffs
Latest
US Treasury's Bessent urges IMF, World Bank to refocus on core missions
U.S.
Wall Street ends higher on earnings, hopes of easing tariff tensions
U.S. stocks rebounded on Tuesday as a spate of quarterly earnings reports and hints at the de-escalation of U.S.-China trade tensions brought buyers in from the sidelines.
See the moment Vatican announces death of Pope Francis

Former CDC official reveals why he left after RFK Jr. took over
CNN's Anderson Cooper speaks with former CDC communications director Kevin Griffis about his decision to step down after President Donald Trump's pick to lead the agency, Robert F. Kennedy Jr., took over.
Trump said he didn’t sign controversial proclamation. The Federal Register shows one with his signature
President Donald Trump downplayed his involvement in invoking the Alien Enemies Act of 1798 to deport Venezuelan migrants, saying for the first time that he hadn’t signed the proclamation, but that he stood by his administration’s move. The proclamation invoking the Alien Enemies Act appears in the Federal Register with Trump’s signature at the bottom. CNN’s Kaitlan Collins reports.
Cory Booker’s historic speech energizes a discouraged Democratic base

Trump's tariffs roil company plans, threatening exports and investment
Businesses around the globe on Thursday faced up to a future of higher prices, trade turmoil and reduced
Stock futures plunge as investors digest Trump’s tariffs
Stock futures plunge as investors digest Trump’s tariffs
Hear Trump break down tariffs on various countries
President Donald Trump announced during a speech at the White House plans for reciprocal tariffs. A group of countries will be charged a tariff at approximately half the rate they charge the United States.
California & Local
See all »L.A. City Council approves proposal to help film production

Ellen Pompeo's star on Hollywood Walk of Fame unveiled

Technology
See all »Meta introduces Llama application programming interface to attract AI developers

JetBlue negotiates partnership with United Airlines, sources say

Brazil's Gerdau remains optimistic about steel orders from the U.S

North Korea conducts first test firing of its new warship's weapons system

Lifestyle
See all »18-wheeler overturns, spills thousands of dimes

Paige Bueckers raised expectations and excitement level for Dallas Wings months before WNBA draft

Store broken into twice in one day

Trump dismisses Biden nominees to US Holocaust Memorial Council, including Doug Emhoff

Entertainment
See all »Electronic Arts lays off hundreds, cancels 'Titanfall' game, Bloomberg News reports

Back on their home courts, Lakers and Rockets are both determined to postpone elimination

Alan Alda had a truly heartfelt moment with Tina Fey at Netflix’s ‘Four Seasons’ premiere

Caesars Entertainment posts narrower first-quarter loss on sports betting surge


 Trump has begun another trade war. Here's a timeline of how we got here
Trump has begun another trade war. Here's a timeline of how we got here
 Canada's leader laments lost friendship with US in town that sheltered stranded Americans after 9/11
Canada's leader laments lost friendship with US in town that sheltered stranded Americans after 9/11
 Chinese EV giant BYD's fourth-quarter profit leaps 73%
Chinese EV giant BYD's fourth-quarter profit leaps 73%
 You're an American in another land? Prepare to talk about the why and how of Trump 2.0
You're an American in another land? Prepare to talk about the why and how of Trump 2.0
 Chalk talk: Star power, top teams and No. 5 seeds headline the women's March Madness Sweet 16
Chalk talk: Star power, top teams and No. 5 seeds headline the women's March Madness Sweet 16
 Purdue returns to Sweet 16 with 76-62 win over McNeese in March Madness
Purdue returns to Sweet 16 with 76-62 win over McNeese in March Madness


