(CNN) — “I was asked to give an update of myself for this documentary, and I wanted to throw up,” Crystal Quigley told CNN.
In a letter dated March 9, Quigley, 39, said she had been sober for two years before relapsing on illicit fentanyl. Her anguish poured out onto the notebook pages she sent us.
“I threw away all I had going for myself because I never felt worthy of my accomplishments,” she wrote. “In true Crystal fashion, I self-sabotaged … all because I didn’t know how to be comfortable sober.”
But the reasons why she relapsed may be more complex.
Two-thirds of Americans say that either they or a family member has been addicted to alcohol or drugs, been homeless because of an addiction, or overdosed and died from drug use. Statistically speaking, addiction has affected the lives of most people reading this. What also may hit close to home with readers is the complicated battle to fight it.
Fentanyl is one of the most powerful synthetic opioids to have infiltrated the street drug supply. Since 2020, fentanyl overdoses have been the leading cause of death for American adults under 50. However, drug overdose death rates that had been soaring since 2018 have begun to drop in at least 45 states, according to the US Centers for Disease Control and Prevention.
Public awareness of its dangers and the distribution of naloxone, a medication that rapidly reverses an opioid overdose, have been credited as reasons for the drop. But overdose death rates are not dropping across all demographics. In fact, they’re still on the rise for certain groups of people.
Nearly a decade into the opioid crisis, new challenges and solutions have emerged. Among them: a growing number of Americans who use illicit fentanyl and survive.
For the past two years, CNN has been documenting illicit fentanyl users, most of whom are in recovery. The adversity they face, both physical and mental, is enormous. What does it even look like to recover from abusing a street drug 50 times stronger than heroin?
These four women shared their stories with CNN for “Fentanyl in America: A Way Out”.
The road to relapse: Crystal Quigley, 39
Crystal Quigley’s substance use started with meth and heroin well over a decade ago. When fentanyl entered the street drug supply, she said, she tried to avoid it.
“I’ve overdosed probably two dozen times” on fentanyl, the 39-year-old said through tears. “My mom found me in the bathroom one time and had to call 911.”
Quigley is a mother of five. Her two boys don’t speak to her. “I still don’t have a relationship with my sons,” she said in 2023. “I know that the person I am now has a fighting chance to get my sons back.”
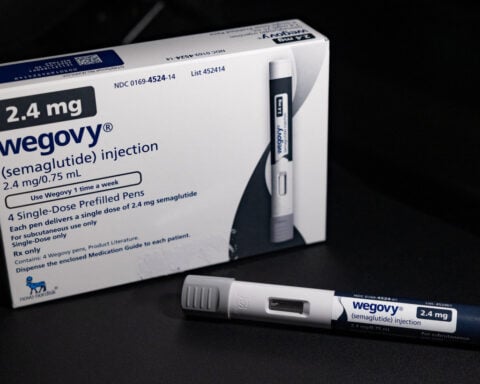
When CNN met her, a year into her sobriety, Quigley credited her success to various forms of buprenorphine, a medication that reduces withdrawal symptoms and curbs cravings for opioids.
She first encountered buprenorphine while incarcerated at Camden County Correctional Facility in south New Jersey, the state’s first jail to offer multiple medications for opioid use disorder.
Quigley started using Sublocade, a monthly injectable form of buprenorphine.
“I’ve been in recovery several times,” she said, “but that shot made me feel more normal than I’ve ever felt in my entire life.”
Buprenorphine has shown to be successful in treating opioid use disorder. In downtown Camden, New Jersey, Cooper University Health Care EMS is the first in the nation to carry buprenorphine, and paramedic Eric Tuttle has seen his share of opioid overdoses.
“We’re probably seeing three to seven overdoses a shift,” he said, and he believes they are mostly caused by illicit fentanyl.
“We’re already precipitating withdrawal with the Narcan [a brand name for naloxone], but we don’t have a choice,” Tuttle said. “The Narcan is needed to get them resuscitated and breathing again.”
Once Tuttle and his team administer Narcan, they offer buprenorphine. “Once you treat the withdrawal, then you can have a nice casual conversation,” he said. As part of that conversation, he offers to take them to the hospital, which will then refer them to an addiction recovery center.
It’s working. Cooper University Health Care conducted a study of its EMTs carrying buprenorphine and found that “the intervention was associated with a nearly sixfold increase in the odds of engagement with treatment within 30 days.” This means administering buprenorphine gives opioid overdose patients a much higher likelihood of getting into an addiction rehabilitation facility.
But buprenorphine has its limits when it comes to illicit fentanyl, according to Dr. Paul Updike, medical director of substance use services at Catholic Health hospital in Buffalo, New York.
Updike finished his medical residency in 1998. “Pretty quickly in my career, I started seeing a lot of patients who were struggling with opioid addiction,” he said.
“Buprenorphine historically did work very well, in my experience, for patients who were using prescription opioids,” he explained. “I personally have hundreds of patients who are on buprenorphine in a maintenance situation.
“As a short-term intervention, buprenorphine is very appropriate and could be very effective. What we’ve been finding, though, because of the potency of fentanyl being so high, is that buprenorphine in the long run is not as effective as it used to be.” In other words, buprenorphine may get you in the door and on your way to recovery, but it may not be what helps you stay.
In October 2023, CNN met Quigley’s two middle-school-age daughters, who seemed delighted to spend time with her. But they struggled to talk about their mother’s substance use.
“The past 15 years with my mom have been like a roller coaster,” Audrena said. “Nights with her not being there, I would just worry her a lot. I was mad at my mom because I didn’t really understand.”
Audrena paused and then said with a maturity well beyond her age: “I’ve realized I shouldn’t be mad at her. It’s a hard thing to overcome. So I just let that be.”
Sitting next to her, Quigley replied, “I was mad, too.”
Months later, after two years on buprenorphine, Quigley would relapse.
Fentanyl while pregnant: Marisa Delles, 26
“What kind of piece of shit uses when they’re pregnant?” 26-year-old Marisa Delles asked. “But it’s reality, and it’s not that simple.”
Delles grew up with an intimate understanding of opioid use. She said her mother became addicted to prescription opioids after a back surgery, although she was reluctant to speak ill of her. “She was pretty normal up until I was 12. … I don’t like talking about all the bad stuff. She definitely did her best. She was a good mom. It was really just when I was older that she started using heroin.”
In Buffalo, New York, where Delles lives, the street drug supply changed well before the Covid-19 pandemic. “You can’t really get heroin anymore. It’s just not really out there,” she said. Illegal fentanyl took its place.
Delles’ mother died of a fentanyl overdose in 2022. “She took a nap, closed her bedroom door, and she was gone,” she said.
At that time, Delles was also using illegal fentanyl. She started using in 2018, when she was 19. After a bad breakup, she said, “I just didn’t want to feel.”
Her use quickly escalated. “I would wake up in the morning, and my legs would be shaking. I would be sweating, and I realized that I need this every day now, and I just never put it down. I was using so much fentanyl a day just to stay unsick, not be shitting myself and throwing up and like rolling around on the floor from withdrawal.”
Withdrawal from fentanyl, according to Delles, is the hardest thing she’s ever gone through. “[Withdrawal] is the number one reason that I never stopped using. … I would beg God to help me get through it. I wanted to be clean so bad, but … it’s too hard.”
Then she became pregnant.
“It’s actually more dangerous to stop using if you’re already pregnant,” said Dr. Lauren Davidson, neonatologist at Sisters of Charity Hospital’s NICU in Buffalo. “The baby can die inside. The baby will also go through withdrawal, much like the mom will if she stops using. And it can cause the baby to actually die in utero.”
Davidson said the number of her patients affected by opioid use disorder has tripled since she started practicing in neonatology. “The more that we judge these mothers,” she said, “it will continue to get worse, because they won’t come for help.”
Delles carried an immense amount of guilt. “I hated myself for getting pregnant,” she said. “Why would I bring a kid into this world … addicted to drugs?”
She used fentanyl for the first three months of her pregnancy, until she found medication to help her wean off. “I definitely had to,” she said. “I couldn’t just quit. I was eating healthy. I was taking my prenatals. I was doing everything that I felt like was going to help.”
She tried a form of buprenorphine called Suboxone, which combines the drug with naloxone, but it was not potent enough, according to Delles. “I was just scrambling to find a way [to stop using fentanyl]. Every day that went by and I was still using was the worst day of my life. They tried putting me on Suboxone, and it didn’t work. I was just rolling around in bed, in withdrawal.”
Then she started methadone treatments and finally stopped using fentanyl. Methadone is a full opioid agonist while buprenorphine is a partial one. To put it simply, it’s a stronger medication. Since the 1960s, methadone has been used as medical treatment for people recovering from heroin use. If she had not found methadone, “I probably would have lost him, or I would have overdosed and died,” Delles reflected. “I don’t even want to think about it. I don’t know how I would have crawled out of this hole.”
Her son, Luca, was born fairly healthy, Delles says.
Like buprenorphine, methadone curbs cravings and eases withdrawal symptoms – and it is partially an opioid, which means Delles’ son would still go through withdrawal symptoms after birth, and he had to stay in the NICU for five days for monitoring. “He only scored a 1 out of 10” on withdrawal severity, Delles says.
No matter the continued risk of withdrawal symptoms, medications like methadone for those who are pregnant are still safer than quitting illicit fentanyl cold turkey, according to Davidson. “It’s monitored,” she said. “It’s not something they’re buying off the street and maybe laced with something that’s even more dangerous and accidentally overdosing and causing both mom and baby to pass.”
Compared with buprenorphine, Updike said, “essentially the patients are sicker, meaning their tolerance is just much higher because of the use of fentanyl” and “methadone is simply more potent.” He believes that it is the most effective treatment for those in recovery from fentanyl abuse.
Delles used methadone for more than two years after her son was born and said she has yet to relapse. But her journey is far from over, according to Updike. “Addiction is very cruel,” he said. “It can kind of lay in wait. You could kind of be doing OK, but life happens. It alters our stress response and people, are just at great risk again.”
Updike believes that most opioid users in recovery from fentanyl should be on methadone for the rest of their lives. “I’m not saying that no patient could be weaned off and remain stable. I’m saying very few. I look at this as the treatment of a chronic illness. It’s not that difficult for me to think of it as not much different than if I was prescribing insulin.”
March 22 was Delles’ last day on methadone.
It’s been over three years since she started treatment, and she believes she’s ready to be done, even though her doctor advised her not to. “It saved my life,” she said. “I wouldn’t ever take it back for anything. But it’s still an opiate. And I think healing my body and my brain is my next step now.” As a new mom, her continued recovery is also motivated by a simple goal for her child. “I just want to give him a normal life,” Delles said.
She credits not just methadone, but a nurse-family partnership program run by Catholic Health hospital in Buffalo. The program supports first-time mothers by helping them with medical care and socioeconomic challenges from pregnancy until their child’s second birthday. Partially because of this program, Delles said, she is in a stable living situation and has graduated from an esthetics program. “You don’t know what you don’t know,” said Delles. “It was night and day. The difference it made.”
This program is funded in part by federal grants, however, and it’s unclear how it might be affected by the Trump administration’s cuts to federal grants and loans.
‘It doesn’t go away’: Jen Gauthier, 39
Jen Gauthier, 39, battled opioid use for over a decade and half. In 2006, she was in a car accident and was prescribed hydrocodone for what she called a minor injury. “Soon as I got that prescription, I felt that euphoria. It was off to the races,” she said.
In 2014, the federal government reclassified hydrocodone as having the highest addiction potential, and it became more restricted. As prescription opioids started to become heavily restricted, they became more expensive to purchase illegally, according to Gauthier. “The heroin is so much cheaper,” she said, “but that was before it all kind of switched over to full-blown fentanyl.”
The difference between heroin and fentanyl is not just strength, but duration of effect. “Fentanyl would not last long,” Gauthier explained. “[It] is out of your system within a couple hours. Within like four hours, you’re sick again.” Like Delles, Gauthier suffered through severe withdrawal until she would use again. “Think of the worst flu that you have ever had and amplify that times 100,” she warned. “It’s brutal.”
For roughly nine years, her life was consumed by illicit fentanyl. Then, also like Delles, she became pregnant.
Gauthier started taking methadone while pregnant with her son, Parker, nearly three years ago and has yet to relapse. “Your brain, everything goes up and down, up and down. And the methadone keeps it level.”
Given how severe and how long her opioid use was, she has no plans to stop the medication. “It doesn’t go away,” she said. “It is still there. I have accepted that whatever I have to do to be sober and be here for my baby and myself, I’m going to do it.”
‘Rotting people’s bodies’: Britiny Mapp, 29
In the most recent data, the CDC reported a nearly 24 percent decline in drug overdose deaths. But the latest CDC data tracking drug overdose deaths by demographic shows that while they are down among White Americans, they continue to go up among Black Americans and Pacific Islanders.
“Being a woman and being of color, I’ve learned that sometimes talking about my experience can help somebody,” said Britiny Mapp, 29.
Mapp is a user in Kensington, Pennsylvania, where a new combination of street drugs entered the market about five years ago: illicit fentanyl combined with sedatives used on animals, known colloquially as “dope” or “tranq.”
“The tranq, that’s a whole different ballgame,” said Mapp, a former student at the Art Institute in Philadelphia. The animal sedatives cause horrific physical damage to users because they restrict blood circulation. “It’s like rotting people’s bodies,” Mapp said. “You got sores all over.”
Mapp said her substance use started after she tore her ACL at age 15 and was prescribed opioids for the pain. In college, she started using heroin. Heroin turned into fentanyl, which turned into tranq.
“I’ve been on methadone,” she explained. “Methadone is only treating the withdrawal from the fentanyl, not the tranq. Tranq is more in like the barbiturate category.” Because tranq is not an opioid, naloxone also doesn’t work in reversing an overdose.
For her, a future in recovery is difficult to picture.
It’s been five years since Mapp started living on the streets in Kensington. In desperation, friends have posted on her Facebook page as recently as February 13: “I miss you, Brit. Contact me. Love you.” “I’ve been thinking of you brit. I hope you’re okay out there.” “Just checking in, hope you’re alright.”
Mapp said she doesn’t look at her Facebook page because it “just gets [her] emotional.” But she knows that her family would “do anything” for her and will be “supportive as possible” whenever she wants to start recovery.
Before the interview ended, she wanted to make one thing clear. “We’re not bad people,” she said. “People don’t give up their children, their homes, their jobs, for no reason. When you put that in perspective, there’s got to be something to it.”
If you or someone you know need help with substance use, call SAMHSA’s National Helpline, 1-800-662-HELP (4357)
The-CNN-Wire
™ & © 2025 Cable News Network, Inc., a Warner Bros. Discovery Company. All rights reserved.

 Trump has begun another trade war. Here's a timeline of how we got here
Trump has begun another trade war. Here's a timeline of how we got here
 Canada's leader laments lost friendship with US in town that sheltered stranded Americans after 9/11
Canada's leader laments lost friendship with US in town that sheltered stranded Americans after 9/11
 Chinese EV giant BYD's fourth-quarter profit leaps 73%
Chinese EV giant BYD's fourth-quarter profit leaps 73%
 You're an American in another land? Prepare to talk about the why and how of Trump 2.0
You're an American in another land? Prepare to talk about the why and how of Trump 2.0
 Chalk talk: Star power, top teams and No. 5 seeds headline the women's March Madness Sweet 16
Chalk talk: Star power, top teams and No. 5 seeds headline the women's March Madness Sweet 16
 Purdue returns to Sweet 16 with 76-62 win over McNeese in March Madness
Purdue returns to Sweet 16 with 76-62 win over McNeese in March Madness