Top Articles

Kings set to face Oilers in round one of Stanley Cup Playoffs: preview

Fyre Festival 2 stops ticket sales for Mexico event
US News
See all »‘The most powerful type of liar’: Tapper asks Anna Delvey how she views her criminal past

Tornadoes, heavy rains rip across central, southern US
Man faces charges after Teslas set on fire with Molotov cocktails

Wisconsin and Florida elections provide early warning signs to Trump and Republicans
World News
See all »Israel to seize parts of Gaza as military operation expands

Middle East latest: Israel is establishing a new military corridor across Gaza
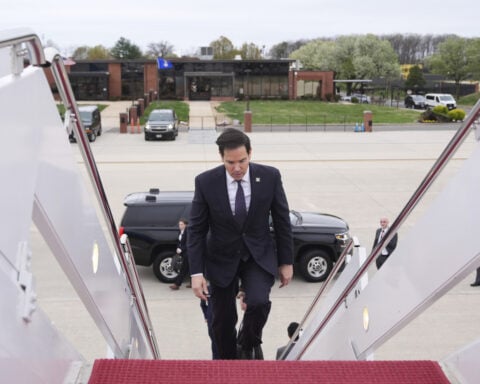
A wary Europe awaits Rubio with NATO's future on the line
China’s military launches live-fire exercise in escalation of blockade drills near Taiwan
Latest
See the moment Vatican announces death of Pope Francis

Former CDC official reveals why he left after RFK Jr. took over
CNN's Anderson Cooper speaks with former CDC communications director Kevin Griffis about his decision to step down after President Donald Trump's pick to lead the agency, Robert F. Kennedy Jr., took over.
Trump said he didn’t sign controversial proclamation. The Federal Register shows one with his signature
President Donald Trump downplayed his involvement in invoking the Alien Enemies Act of 1798 to deport Venezuelan migrants, saying for the first time that he hadn’t signed the proclamation, but that he stood by his administration’s move. The proclamation invoking the Alien Enemies Act appears in the Federal Register with Trump’s signature at the bottom. CNN’s Kaitlan Collins reports.
Cory Booker’s historic speech energizes a discouraged Democratic base

Trump's tariffs roil company plans, threatening exports and investment
Businesses around the globe on Thursday faced up to a future of higher prices, trade turmoil and reduced
Stock futures plunge as investors digest Trump’s tariffs
Stock futures plunge as investors digest Trump’s tariffs
Hear Trump break down tariffs on various countries

Attorney for father deported in 'error' says this is what's 'new, unique and terrifying' about case
CNN's Erin Burnett speaks with Simon Sandoval-Moshenberg, the attorney for a Maryland father the Trump administration conceded it mistakenly deported to El Salvador “because of an administrative error.”
Federal judge to consider case of Georgetown fellow arrested by ICE
Federal judge to consider case of Georgetown fellow arrested by ICE
Canadian couple cancels tens of thousands in travel to the US
CNN's Natasha Chen spoke to Gary and Carol Cruise who normally spend a small fortune traveling throughout the US every year. Because of remarks by President Donald Trump and the tariff war, they've cancelled nearly everything.
California & Local
See all »Pope Francis dies at the Vatican at age 88

Kings set to face Oilers in round one of Stanley Cup Playoffs: preview

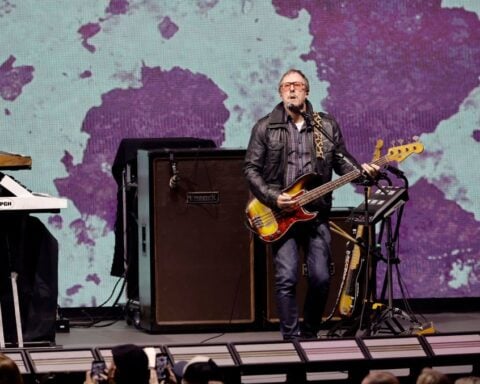
Weezer bassist to play Coachella despite wife’s arrest
Technology
See all »Walmart-backed Flipkart to shift base back to India from Singapore

China's Nio delays Europe launch of Firefly EV to third quarter

Crowd roars over question about what oversights Byron Donalds would impose on Elon Musk and DOGE

Buyout firm Thoma Bravo nears deal for Boeing's Jeppesen unit, Bloomberg News reports

Lifestyle
See all »Viral TikTok "Miracle Tree" draws hundreds seeking healing and hope

Timothée Chalamet’s mother, Nicole Flender, is having her own moment

Wendy's raising money to support Ohio woman who lost friend and home after tree collapse
Entertainment
See all »Bryce Dallas Howard says she went into ‘momager’ mode for dad Ron Howard’s cameo on ‘The Studio’

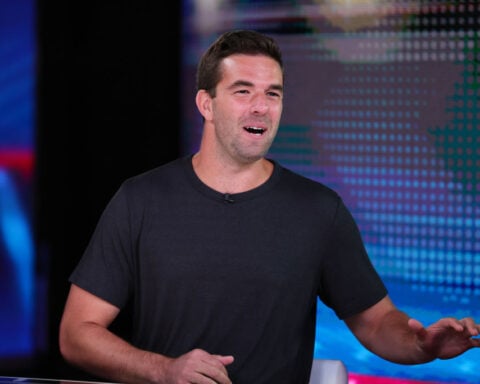
Pro Football Hall of Famer and podcast star Shannon Sharpe sued for sexual assault and battery

Pedro Pascal is a very busy man. Where you can watch ‘The Last of Us’ star next

Timothée Chalamet’s mother, Nicole Flender, is having her own moment


 Trump has begun another trade war. Here's a timeline of how we got here
Trump has begun another trade war. Here's a timeline of how we got here
 Canada's leader laments lost friendship with US in town that sheltered stranded Americans after 9/11
Canada's leader laments lost friendship with US in town that sheltered stranded Americans after 9/11
 Chinese EV giant BYD's fourth-quarter profit leaps 73%
Chinese EV giant BYD's fourth-quarter profit leaps 73%
 You're an American in another land? Prepare to talk about the why and how of Trump 2.0
You're an American in another land? Prepare to talk about the why and how of Trump 2.0
 Chalk talk: Star power, top teams and No. 5 seeds headline the women's March Madness Sweet 16
Chalk talk: Star power, top teams and No. 5 seeds headline the women's March Madness Sweet 16
 Purdue returns to Sweet 16 with 76-62 win over McNeese in March Madness
Purdue returns to Sweet 16 with 76-62 win over McNeese in March Madness

