Top Articles

California poll reveals widespread support for immigrant social service access

LA28 unveils updated Olympic venue plan

US News
See all »‘The most powerful type of liar’: Tapper asks Anna Delvey how she views her criminal past

Tornadoes, heavy rains rip across central, southern US
Man faces charges after Teslas set on fire with Molotov cocktails

Wisconsin and Florida elections provide early warning signs to Trump and Republicans
World News
See all »Israel to seize parts of Gaza as military operation expands

Middle East latest: Israel is establishing a new military corridor across Gaza
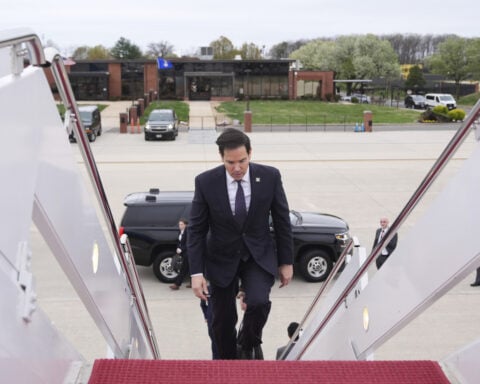
A wary Europe awaits Rubio with NATO's future on the line
China’s military launches live-fire exercise in escalation of blockade drills near Taiwan
Latest
Cory Booker’s historic speech energizes a discouraged Democratic base

Trump's tariffs roil company plans, threatening exports and investment
Businesses around the globe on Thursday faced up to a future of higher prices, trade turmoil and reduced
Stock futures plunge as investors digest Trump’s tariffs
Stock futures plunge as investors digest Trump’s tariffs
Hear Trump break down tariffs on various countries

Attorney for father deported in 'error' says this is what's 'new, unique and terrifying' about case
CNN's Erin Burnett speaks with Simon Sandoval-Moshenberg, the attorney for a Maryland father the Trump administration conceded it mistakenly deported to El Salvador “because of an administrative error.”
Federal judge to consider case of Georgetown fellow arrested by ICE
Federal judge to consider case of Georgetown fellow arrested by ICE
Canadian couple cancels tens of thousands in travel to the US

Europe prepares countermeasures to Trump’s tariffs, calling them a ‘major blow to the world economy’
Europe prepares countermeasures to Trump’s tariffs, calling them a ‘major blow to the world economy’
Exclusive: Secretary of Education explains what department will do after Trump begins dismantling it
Secretary of Education Linda McMahon outlines what she expects the Department of Education will do now following President Donald Trump's executive order that began the process of dismantling the department.
Former federal judge says Trump is playing a 'dangerous game' with Judge Boasberg
Former federal judge John E. Johns III responds to White House Deputy Chief of Staff Stephen Miller, who said judges have no authority to administer the Executive Branch. Jones also explains why he believes President Donald Trump and his administration are playing a dangerous game by attacking Judge Boasberg.
California & Local
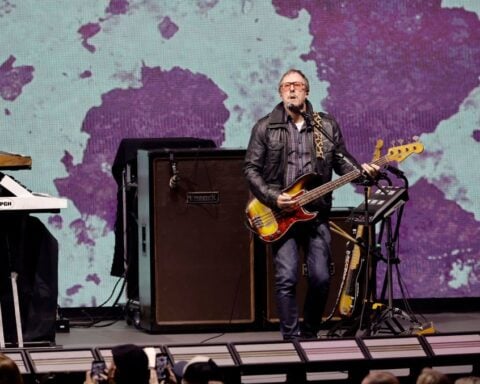
See all »Weezer bassist to play Coachella despite wife’s arrest
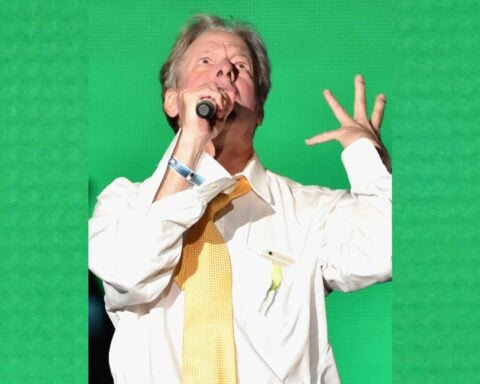
KROQ DJ Jed 'The Fish' Gould dies at 69
Technology
See all »Scientists find possible chemical signs of life on a faraway planet
Google's digital ad network declared an illegal monopoly, joining its search engine in penalty box

Google is an online advertising monopoly, judge rules

Scientists detect signature of life on a distant planet, study suggests

Lifestyle
See all »NJ pet owner searching for lost dog last seen going under fence into restricted Naval base

Limited-edition Boston Marathon bracelets encouraging egg hunt around city

A restaurant in Havana defies Cuba's tech struggles with digital menus and a robot waitress

Believers say microdosing psychedelics helps them. Scientists are trying to measure the claims

Entertainment
See all »Drake complains about Kendrick Lamar's 'Not Like Us' Super Bowl performance in new defamation claims

Dozens more possible jurors are screened in Weinstein retrial

Lee Corso to retire from ESPN's 'College GameDay' after four-decade run

Iconic ESPN broadcaster Lee Corso to retire from ‘College Gameday’


 Trump has begun another trade war. Here's a timeline of how we got here
Trump has begun another trade war. Here's a timeline of how we got here
 Canada's leader laments lost friendship with US in town that sheltered stranded Americans after 9/11
Canada's leader laments lost friendship with US in town that sheltered stranded Americans after 9/11
 Chinese EV giant BYD's fourth-quarter profit leaps 73%
Chinese EV giant BYD's fourth-quarter profit leaps 73%
 You're an American in another land? Prepare to talk about the why and how of Trump 2.0
You're an American in another land? Prepare to talk about the why and how of Trump 2.0
 Chalk talk: Star power, top teams and No. 5 seeds headline the women's March Madness Sweet 16
Chalk talk: Star power, top teams and No. 5 seeds headline the women's March Madness Sweet 16
 Purdue returns to Sweet 16 with 76-62 win over McNeese in March Madness
Purdue returns to Sweet 16 with 76-62 win over McNeese in March Madness